Concussion Care in Urgent Care Centers and Emergency Departments
Learn how to manage concussions in the urgent care and emergency department settings using evidence-based and clinically proven tools and methodologies.
Benefits of Concussion Assessment in an Urgent Care Clinic
Immediate: Similar to emergency department care, providers in the urgent care setting typically see patients as close to the time of their injury as relevantly possible, oftentimes the same day.
Accessible: Urgent cares are often open during the evening, weekends, and holidays, when primary doctors offices are typically closed. Their locations also tend to be widespread, particularly in metropolitan areas.
Reimbursable: Earn up to $250 in reimbursement per concussion evaluation.
Concussion Education
It’s important to understand and educate your patients on the current state of concussion knowledge in order to guide them away from misinformation.
Here are a few concussion facts to go over with your patients:
- Concussion is a non-structural injury.
- Concussions are not graded or ranked.
- Scans and imaging do not effectively show concussions.
Urgent Care vs ER: When does a head injury require an emergency department visit?
The patient should be sent to the emergency department for a closed head injury if they require immediate, high-level imaging.
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) can be used to assess the patient to decide whether they can be seen in the urgent care setting or whether they require a higher level of medical attention.
Eye Opening Response
- Spontaneous--open with blinking at baseline: 4 points
- To verbal stimuli, command, speech: 3 points
- To pain only (not applied to face): 2 points
- No response: 1 point
Verbal Response
- Oriented: 5 points
- Confused conversations, but able to answer questions: 4 points
- Inappropriate words: 3 points
- Incomprehensible speech: 2 points
- No response: 1 point
Motor Response
- Obeys commands for movement: 6 points
- Purposeful movement to painful stimulus: 5 points
- Withdraws in response to pain: 4 points
- Flexion in response to pain (decorticate posturing): 3 points
- Extension response in response to pain (decerebrate posturing): 2 points
- No response: 1 point
Deductions on the Glasgow Coma Scale may indicate the need for the patient to go to the emergency department.
Canadian CT Head Rule Criteria
The Canadian CT Head Rule (CCHR) is an evidence-based clinical decision rule to determine when a head CT is necessary. If any of the following conditions are met, it would indicate that the patient should go to the ER for a head CT.
- A Glasgow Coma Scale score of less than 15, two hours after the injury
- Suspected open or depressed skull fracture
- Any sign of basilar skull fracture: hemotympanum, raccoon eyes (intraorbital bruising), battle sign (retroauricular bruising), or cerebrospinal fluid leak, oto- or rhinorrhea
- Two or more episodes of vomiting
- 65 years of age or older
- Amnesia for events occurring more than 30 minutes prior to impact
- Dangerous mechanism of injury (e.g. pedestrian struck by motor vehicle, occupant ejected from motor vehicle, fall greater than 3 feet, fall downstairs more than 5 steps)
New Orleans Criteria
The New Orleans Criteria (NOC) is another evidence-based clinical decision rule to determine when a head CT is necessary. The criteria includes a Glasgow Coma Scale of 15 and any of the following:
- Headache
- Vomiting
- Age greater than 60
- Drug or alcohol intoxication
- Persistent anterograde amnesia
- Seizure
- Visible trauma above the clavicle
Nexus II Criteria
Nexus II is another evidence-based clinical decision making tool that can be used to help determine when a patient should go to the emergency room. The criteria includes any of the following:
- Skull fracture
- Scalp hematoma
- Neurologic deficit
- Altered level of alertness
- Abnormal behavior
- Coagulopathy
- Persistent vomiting
Each of the decision making rules should be used as guidelines and will require provider discretion and clinical decision making to determine whether or not it is appropriate to send the patient to the ER. These evidence-based rules can also be used to support your clinical decision making and should be included in your documentation.
Who is on the concussion care team?
The first step in setting up your concussion care team is determining a point person. This is typically a physician, ideally a Credentialed ImPACT Consultant (CIC), who is knowledgeable on the management of concussions. Additionally, the concussion care team may consist of nurse practitioners, physician assistants, medical assistants, athletic trainers, physical therapists, and other specialists.
Emergency Department / Urgent Care Concussion Evaluation
History:
Obtain a detailed mechanism of injury (MOI) from the patient and any eyewitnesses. Gathering multiple accounts of what happened will help provide a fuller picture of what occurred.
Ask eyewitnesses:
Was the patient confused?
Was their balance off?
Did they seem nauseous, lightheaded, dizzy, or wanting to vomit?
Was their memory immediately impaired?
Assess for amnesia both prior to the injury as well as after the injury.
To assess for retrograde amnesia, ask the patient about details of their day leading up to the injury.
What quarter or half did the injury occur?
What was the score?
Was it a home or away game?
Did you have a pregame meal or snack?
Did you travel to the game?
To assess for anterograde amnesia, ask the patient details about their evaluation immediately after the head injury.
Who evaluated you?
Did you continue to participate in the event or where you pulled out?
What was the final score of the game?
Use eyewitness accounts to cross-reference the patient’s recollection of events before and after the head injury.
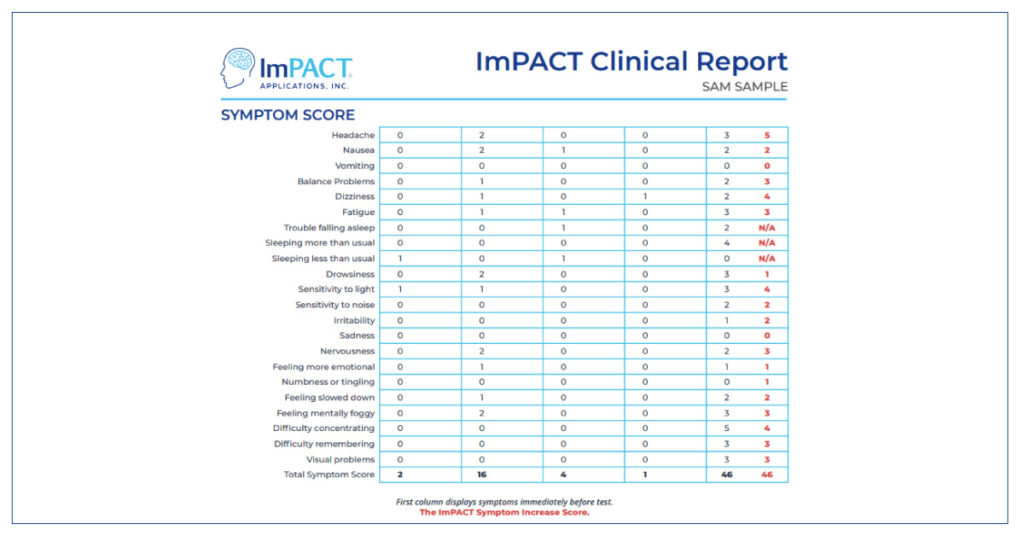
Symptom Evaluation:
Next, review any associated symptoms. You may consider using a graded or scaled symptom checklist such as the ImPACT Post-Concussion Symptom Scale to monitor symptoms from the initial evaluation throughout recovery.
Additionally, here are some common questions to ask the patient about their symptoms:
Do you have a pressure in your head that increases as the day progresses?
Do you feel more fatigued than normal at the end of the day?
Do busy environments cause you to feel foggy, anxious, tired?
Do you become dizzy when looking up/down, turning your head, or standing quickly?
Do you have blurred or fuzzy vision while reading or difficulty reading?
Do you feel a frontal pressure in your head when reading or on the computer?
Do you feel more distractible than normal?
Are you having more difficulty watching films or reading the playbook?
Do you have difficulty falling/staying asleep?
Have you or your family noticed changes in mood such as irritability or anxiety?
Physical Exam:
At a minimum, your physical exam should include:
- General observation (gait, blank stare, attention, delayed responses, emotionality, interaction with others)
- Checking cranial nerves 2-12
- Motor exam including strength
- Sensory exam
- Rhomberg testing
Cognitive Evaluation:
At a minimum, the cognitive assessment should include:
- Orientation - Is the patient oriented to the date, month, year, time, etc.?
- Memory - 5-10 word memory recall (3 sets)
- Concentration - 3-6 digits repeated back in reverse
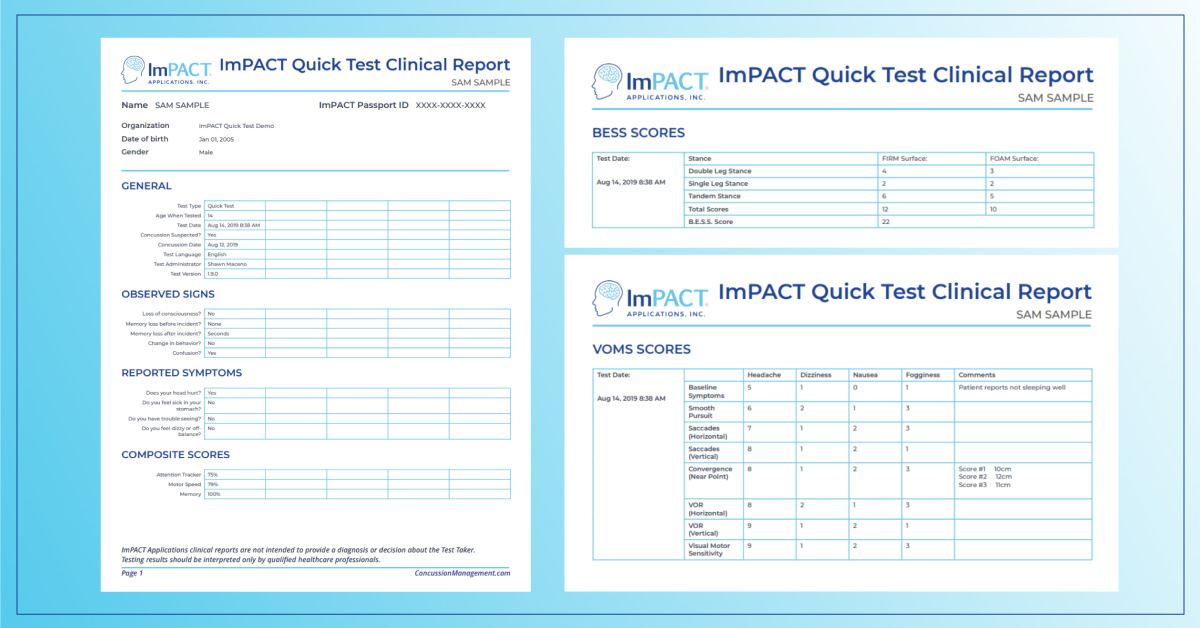
BESS:
The Balance Error Scoring System (BESS) is a rather simple balance test that can be done in the office, requiring only a foam pad, timer, and someone to act as a spotter.
The patient’s balance is tested on two different surfaces: a hard floor surface and a softer foam surface. On each surface, the patient is taken through 3 stances: double leg stance, single leg stance, and tandem stance. The patient’s balance is tested for 20 seconds in each stance on each surface.
BESS errors include:
- Hands lifted off iliac crest
- Opening eyes
- Step, stumble, or fall
- Moving hip into > 30 abduction
- Lifting forefoot or heel
- Remaining out of test position > 5 seconds
The final score is calculated by adding one point for each error during the 6 tests.
VOMS:
Vestibular Ocular Motor Screening (VOMS) is a vestibular ocular test that can be completed in about 5-10 minutes.
First, you’ll measure their baseline of the following symptoms on a scale of 0-10:
- Headache
- Dizziness
- Nausea
- Fogginess
Then, you’ll take the patient through the following tests, reassessing their symptoms after each:
- Smooth pursuits
- Saccades (horizontal and vertical)
- Near point convergence
- Vestibular ocular reflex (horizontal and vertical)
ImPACT:
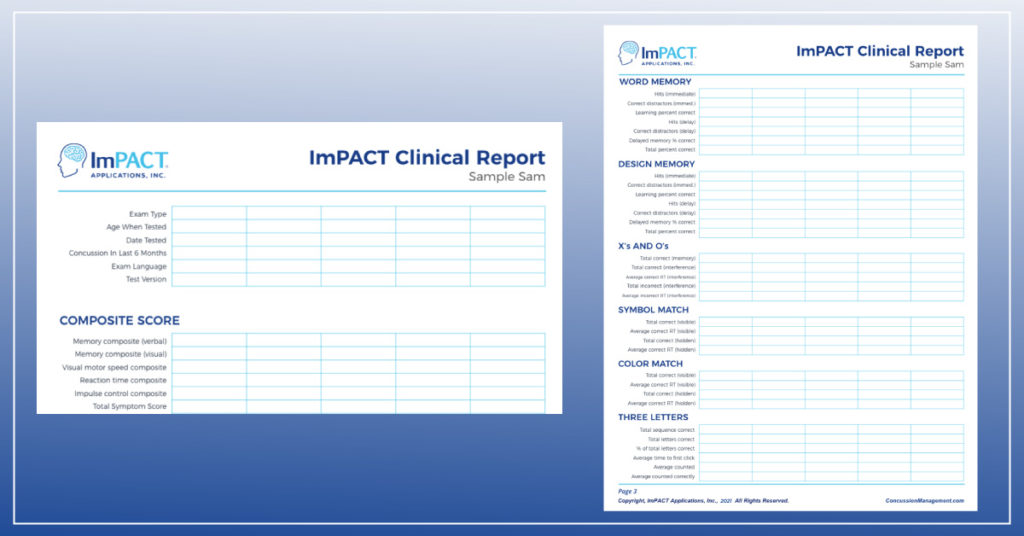
ImPACT is a computerized neurocognitive test administered on a desktop or laptop computer in about 20 minutes. It includes both baseline and post-injury tests and is used to track patients cognitive status throughout recovery until they return to baseline. If no baseline exists for the patient, normative data is available.
After ImPACT is completed, a clinical report is generated which includes details in regards to the injury such as concussion date, exam date, age of the patient when tested, as well as their composite scores. In addition, it includes breakdowns of how they performed in each section: word memory, design memory, X’s and O’s, symbol matching, color match, and three letters.
ImPACT Quick Test:
ImPACT Quick Test is administered on an iPad in 5-7 minutes and is used at the point of care to determine if a patient should be further evaluated for concussion. It also includes the ability to record VOMS and BESS evaluations.
After ImPACT Quick Test is completed, a clinical report is generated that includes composite scores for attention tracking, motor speed, and memory. It also includes sections for their observed signs and reported symptoms as well as for BESS and VOMS, if administered.
Determining a Clinical Trajectory
The history, physical exam, ImPACT scores, VOMS, and patient’s symptoms can all be used in conjunction to help determine a clinical trajectory.
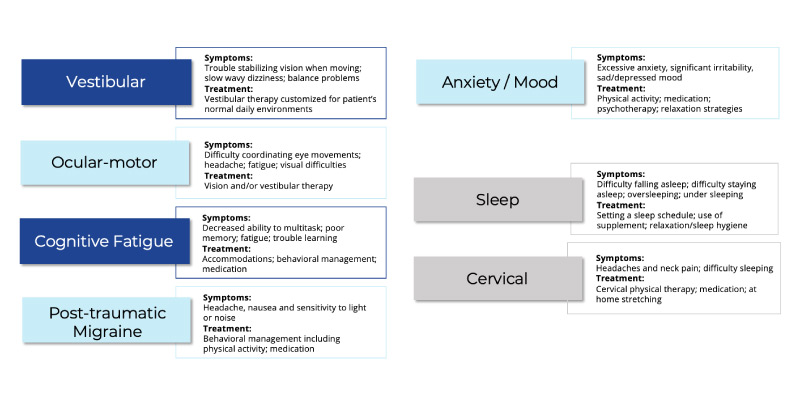
The 5 clinical trajectories include:
- Vestibular
- Ocular
- Cognitive fatigue
- Post-traumatic migraine
- Anxiety / Mood
Additionally, there are 2 clinical modifiers which can affect any of the trajectories: sleep and cervical.
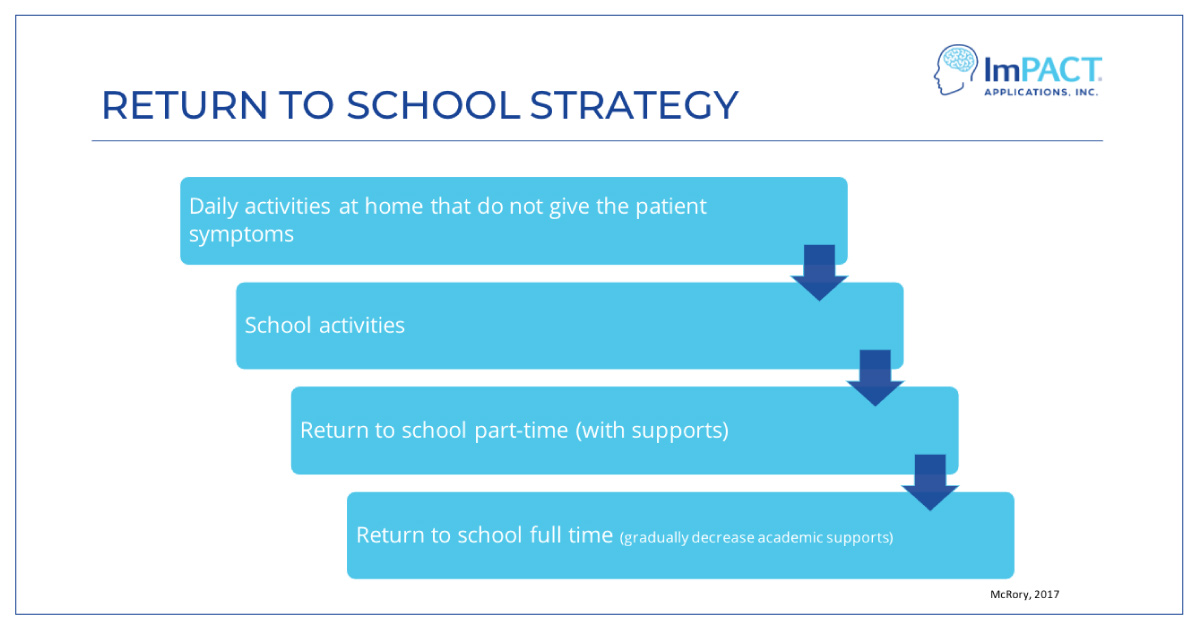
Graduated Return to School
If your patient is a student, follow this 4 step graduated return to school program.
Stage 1: No activities that provoke symptoms (e.g. screen time)
Stage 2: School activities outside of the classroom that do not aggravate symptoms (e.g. homework, reading, other cognitive tasks)
Stage 3: Return to school part-time
Stage 4: Return to school full time
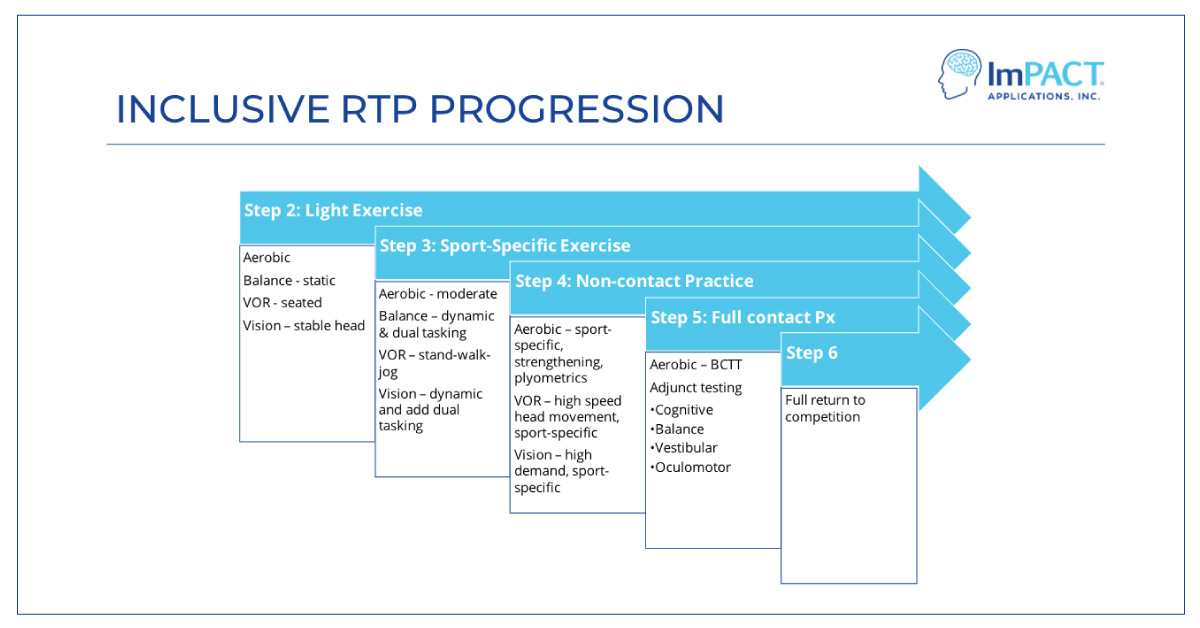
Graduated Return to Activity
If your patient is an athlete, follow this 6 step graduated return to activity progression.
Stage 1: No activities that provoke symptoms (e.g. PE; weightlifting)
Stage 2: Light aerobic exercise (e.g. walking; stationary bike at medium pace)
Stage 3: Sport-specific exercise (e.g. running; skating drills)
Stage 4: Non-contact training drills specific to their sport (e.g. passing drills; resistance training)
Stage 5: Full contact practice
Stage 6: Return to sport and normal game play
Symptoms should be monitored at each stage of the return to play progression, ensuring patients are remaining asymptomatic when moving from one stage to another.
Reimbursement
Earn up to $250 in reimbursement per concussion evaluation using ImPACT or ImPACT Quick Test. Learn more about reimbursement for concussion care services in the billing guide.
Sources:
https://idph.iowa.gov/Portals/1/Files/ACBI/BESS%20manual%20310.pdf
https://pubmed.ncbi.nlm.nih.gov/11356436/
https://pubmed.ncbi.nlm.nih.gov/10891517/
https://pubmed.ncbi.nlm.nih.gov/16374287/
https://pubmed.ncbi.nlm.nih.gov/28446457/
https://www.physiotherapyalberta.ca/files/vomstool.pdf
https://pubmed.ncbi.nlm.nih.gov/24337463/
Want to learn more?
Download this guide and take the video-on-demand course
Concussions in Urgent Care.
Leave your email below and we'll send you the PDF and a link to take the course for free.
Concussion Care in Urgent Care Centers LP Email Course Promo Code